Less Pain, Greater Mobility The Power Of Fascia Fitness
2024-08-14
After teaching at top national conferences recently, probably the biggest question I got was in regard to the topic of fascia. I’ll admit, there is ALL sorts of information around the topic of fascia in fitness nowadays and it can be very confusing and overwhelming.

I know this because I first learned about fascia in the late 1990’s (dating myself here) after reading renowned physical therapist, Diane Lee’s book “The Pelvic Girdle”. In this great book, Ms. Lee breaks down some fascinating research that began with leading scientist and therapist, Dr. Andry Vleeming.

It took me a while to really figure out what to do with the information I was reading because at the time NO ONE was talking about fascia in training. Looking back, there were some key concepts I wish I had taken away which are…
-There are many different types of fascia in our body and they can play a wide variety of roles.
-Some of these roles include force transmission from one area of the body to another.
-Stabilization of joints while we perform everyday movements that we often think are simple but are quite complicated, like locomotion.
These base concepts help us understand how much the body is interconnected and even when a muscle contracts, it doesn’t do so by itself. I’ll admit, this is an oversimplification of a very complex topic, but I always look for what is usable information in training.
In understanding fascia better I want people to see how we can help issues of reducing pain, improving mobility, and developing greater strength in our training.
Decrease Pain
Even the medical community used to think fascia wasn’t all that useful (mostly referring to superficial fascia). Since then, many surgeons have been even more careful about the impact they make to the fascia while they perform various surgeries because they realize it impacts healing and future pain and movement.
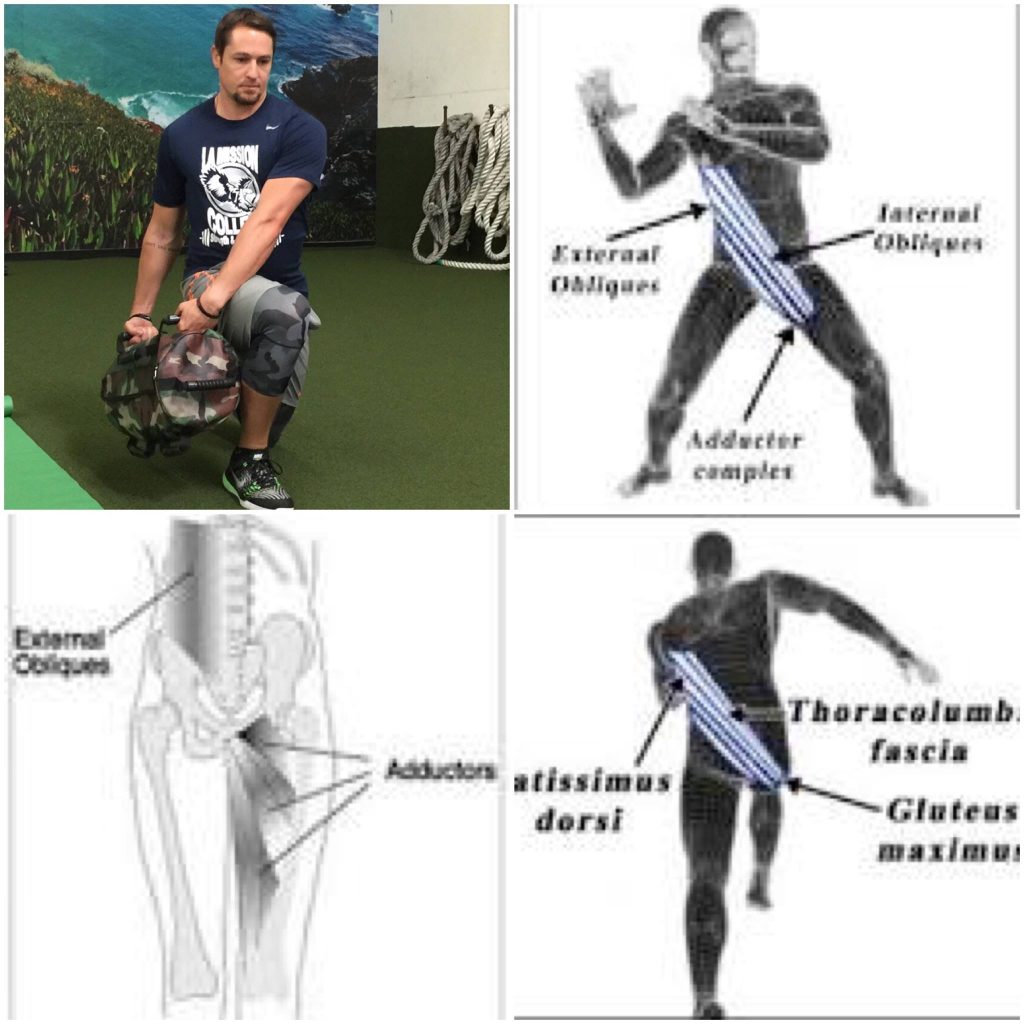
Most people are unaware that fascia has 250 million nerve endings and pain receptors, compared to the skin which has 200 million and the eyes have 126 million visual receptors. That means the pain we experience can have fascial influencers.
As fascial expert, Dr. Helene Langevin explains, “Patients with connective tissue hyper- and hypo-mobility disorders suffer in large number from musculoskeletal pain, and many have abnormal proprioception. The relationships among fascia mobility, proprioception, and myofascial pain are largely unstudied, but a better understanding of these areas could improve care for many patients with musculoskeletal pain.” (1)
It is estimated that around 30% with chronic musculoskeletal pain in the back, neck, shoulder, hip, pelvis and headaches are due to issues of the fascia and muscle (2). Both the nerves of the fascia and the movement capability of the fascia can impact both mobility and pain experiences. When fascia is not moving efficiently we often can see increases in pain and that is why we will explore how movement plays a big part in how we can make fascia healthier.
Improve Mobility
Many times when we have a new client come into the gym, especially if they have not been very physically active, they will be explaining how they feel quite “tight” in a variety of areas of the body. This isn’t because they are not warmed up or haven’t been moving much throughout the day. The reality is that our fascia can start to change its structure the less we move and when we move in less diverse ways (1). You may see how natural it is for us to try to move when we have been resting if you have ever watched your dog or cat wake up and the first thing they do is stretch!
In a time where people are more sedentary, it should be no surprise that people have more restricted movement capabilities and we are seeing increased issues of aches/pains. A key aspect in improving our mobility is making sure our fascia is moving as well as possible. This means incorporating more of what has fallen out of favor which is stretching.
As Dr. Langevin explains, “We know that fascia can become inflamed and transmit pain signals. We also know that even minor injuries can cause adhesions in the fascia, which mean the layers of this tissue may become “stuck” and lose their ability to glide as they do in healthy connective tissue. These issues can accumulate, with pain leading to reduced mobility and activity, and reduced mobility and activity contributing to worsening pain, resulting in a persistent cycle of deterioration or exacerbation.” (3)
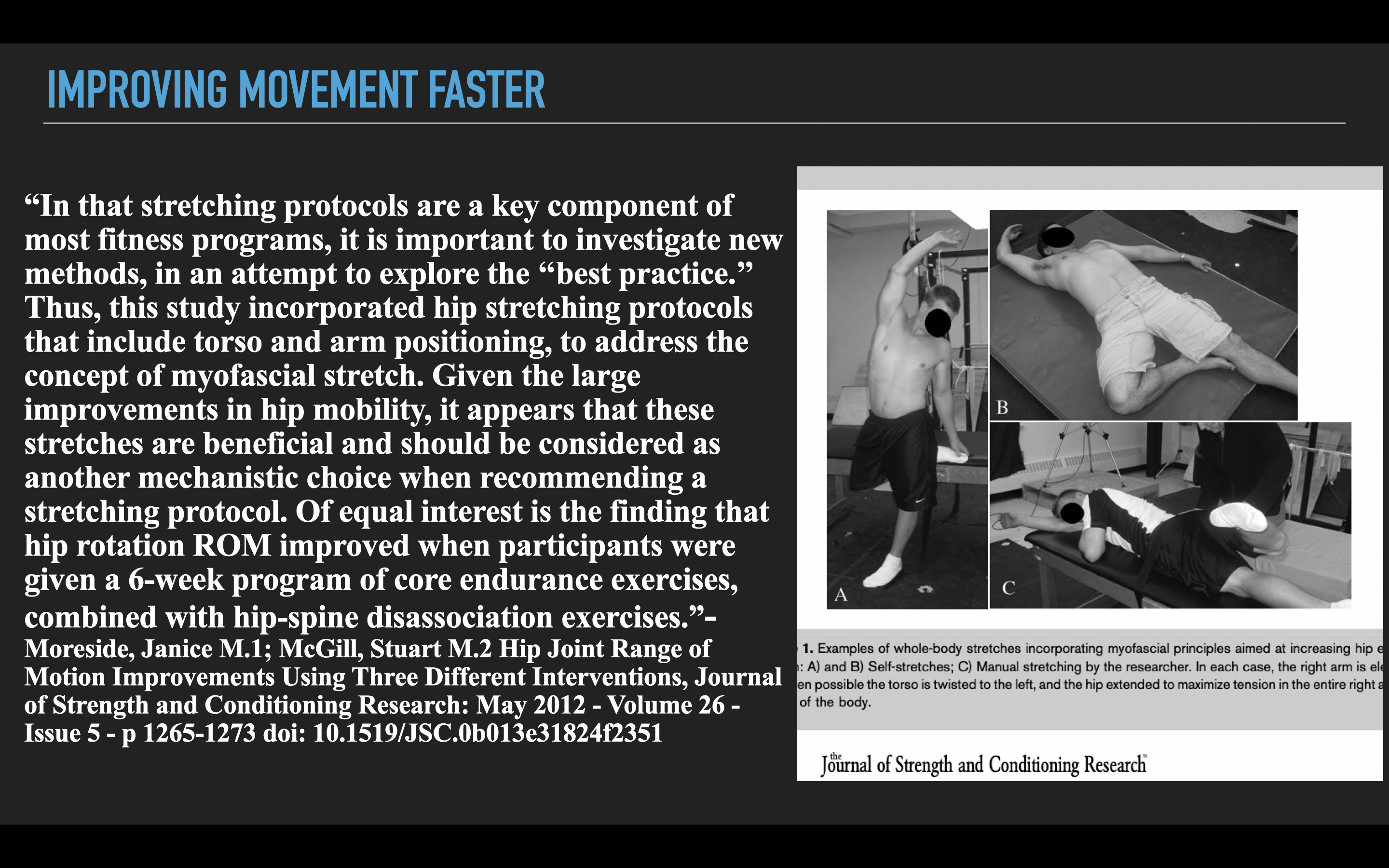
Stretching holds more value than we may have thought as Dr. Langevin continues, “Research in animal models has shown that stretching has anti-inflammatory effects in several types of inflammation, and we need to understand better if this holds true in humans.”
Now, if you are terrified that you will stretch and become weak for your workouts, there is great new evidence to be aware of such as a 2007 paper in Sports Medicine that states, “Although most studies have found acute decreases in strength following stretching, and that such decreases seem to be more prominent the longer the stretching protocol, the number of exercises and sets, and the duration of each set have, in general, exceeded the ranges normally recommended in the literature. Consequently, the duration of the stimuli were excessively long compared with common practice, thus making evident the need for further studies.” (4)
Additional studies have gone on to point out that when we perform very long duration stretches (those of well over 30 seconds at a time) this is where we see greatly decreased strength. However, they also note that almost no one actually stretches in this manner, and much shorter durations of negligible effect on strength performance (5). If we also figure in the idea that we can reduce pain sensations and increase movement of the body it makes sense that we refocus on these concepts of stretching again.
We should look at how to make our stretching more efficient and effective. There are several things we should consider…
-Using deep breathing can improve the effectiveness of stretching compared to just stretching without the intentional breath work (6).
-Meditative movement practices (like we show in the video below) have a significant impact on the mobility of the body through both fascia and muscle (7).
-Such meditative movement practices also address aspects of the biopsychosocial model that have a profound impact on pain, reducing tightness by relaxing the autonomic nervous system, and learning to relax the body (8).
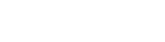
The following movements show how we can address more full body mobility and the influence of the fascial slings that connect throughout our body. In an upcoming post we will discuss the influence of fascia to strength but hopefully you are seeing how if we understand fascia we can make greater impacts upon movement, health, and overall well-being.
Find out more in with our Myofascial Integrated Movement programs 35% off with code “mim35” HERE
References:
- Langevin, H.M. Fascia Mobility, Proprioception, and Myofascial Pain. Life 2021, 11, 668. https://doi.org/10.3390/life11070668
- Fricton, J. Myofascial pain: Mechanisms to management. Oral. Maxillofac. Surg. Clin. N. Am. 2016, 28, 289–311
- https://www.nccih.nih.gov/research/blog/more-stretching-less-stressing
- Rubini, Ercole C., André LL Costa, and Paulo SC Gomes. “The effects of stretching on strength performance.” Sports medicine 37 (2007): 213-224.
- Ryan, Eric D., et al. “Do practical durations of stretching alter muscle strength? A dose-response study.” Medicine & Science in Sports & Exercise 40.8 (2008): 1529-1537.
- Lamontagne, Emilie, and Trevor G. Cottrell. “A Comparison of the Effects of Static Stretching Alone to Static Stretching Plus Slow Deep Breathing on Hip Flexion Range of Motion.” (2021).
- Wehner C, Wehner C, Schwameder H, Schobersberger W. Thoracolumbar Rotation During Tai Chi Movements-A Biomechanical Analysis of the Entire Peking Style Routine. Front Sports Act Living. 2022 Feb 2;4:834355. doi: 10.3389/fspor.2022.834355. PMID: 35187479; PMCID: PMC8849243.
- Wehner C, Wehner C, Schwameder H, Schobersberger W. Thoracolumbar Rotation During Tai Chi Movements-A Biomechanical Analysis of the Entire Peking Style Routine. Front Sports Act Living. 2022 Feb 2;4:834355. doi: 10.3389/fspor.2022.834355. PMID: 35187479; PMCID: PMC8849243.
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.