Exercise To Fight Chronic Inflammation & Improve Results
2024-09-11
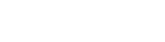
One concept everyone seems to agree is bad (which is amazing in today’s world) is chronic inflammation. When we experience chronic inflammation it becomes a breeding ground for many different health issues to develop. There are many different mechanisms this can occur, but it causes havoc on all the systems of our body. Since everything in our body is connected, when you impact one system (like our immune system for example) you impact the other systems of the body.
The question becomes how can we avoid chronic inflammation, to be honest, none of it is going to be very complicated or possibly earth shattering. That doesn’t mean they are necessarily easy to accomplish because it has all to do with lifestyle.
Yet, let me share some really intriguing current concepts around chronic inflammation that you may find very profound and encourage you to find ways to implement what I will suggest. There is a rather new field of study called, psychoneuroimmunology, which looks at how our emotional state impacts our nervous system and then influences our immune system.
When we have chronic stress occurring in our lives (this can come in various forms as I will explain) it can lead to sickness behavior. This is where, stay with me here….
“Anyone who has experienced an episode of viral or bacterial infection knows well the subjective feelings of sickness, in the form of malaise, lassitude, fatigue, numbness, coldness, muscle and joint aches, and reduced appetite. Because they are common, these symptoms usually are ignored by physicians. They are considered uncomfortable, but banal, components of the pathogen-induced debilitation process that affects sick individuals.
This simplistic view has turned out to be incorrect. The psychologic and behavioral components of sickness represent, together with fever response and associated neuroendocrine changes, a highly organized strategy of the organism to fight infection [1]. This strategy, referred to as “sickness behavior,” is triggered by the proinflammatory cytokines produced by activated cells of the innate immune system in contact with specific pathogen-associated molecular patterns (PAMPs). These cytokines include mainly interleukin (IL) 1 (IL-1α and IL-1β), IL-6, and tumor necrosis factor α (TNF-α).” (1)
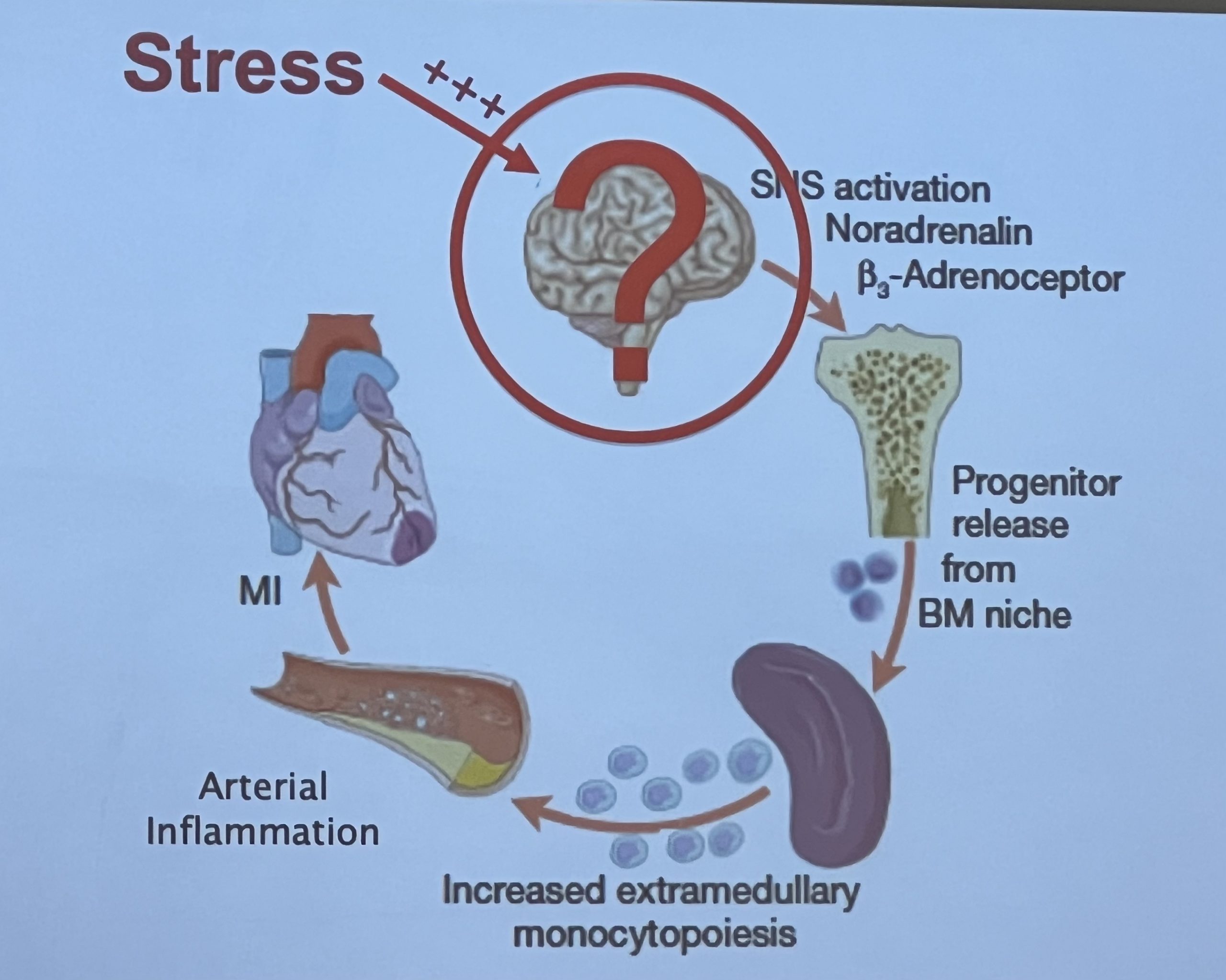
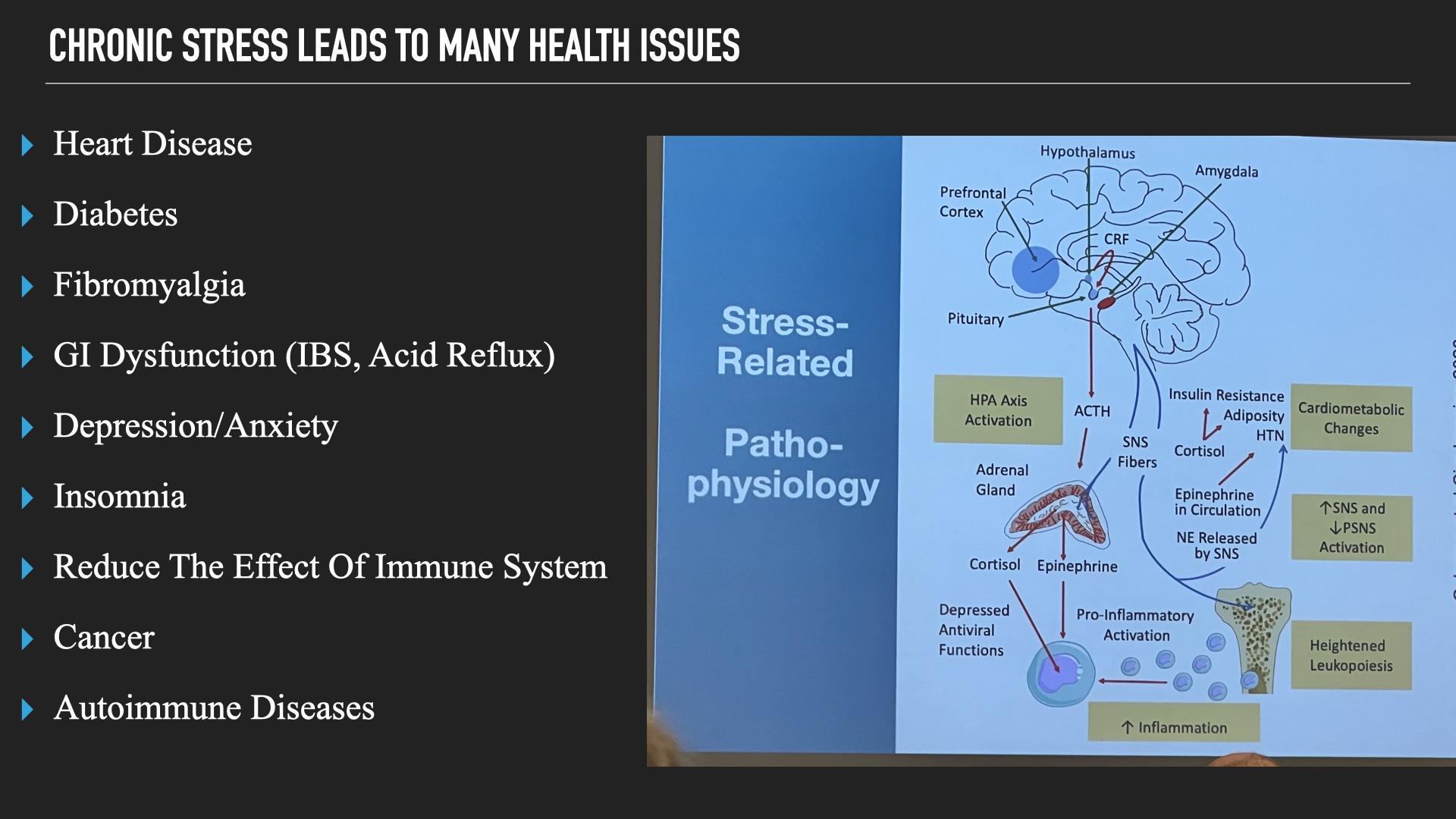
This information was provided at Harvard Medical School’s symposium on whole person health. Explaining some of the mechanisms of how stress which leads to chronic inflammation contributes to cardiovascular disease.
What is important to note here is that our psychology and behavior are often altered when our brain believes we are fighting something when pro inflammatory cytokines rely this information to our brain. In short bouts when we are sick that is fine, but the issue is when we are under chronic stress our brain starts to think we are constantly fighting something and that is where fatigue, depression, overeating (whether to help sooth our discomfort or our brain thinks we need more energy than we actually do) and many other mental health issues can stem from.
Reducing chronic inflammation therefore lowers these proinflammatory cytokines. While many fitness pros only focus on eating healthy, exercise, and sleep (which are all helpful) they ignore situations in people’s worlds that negatively impact the previous three habits. As renowned neuroscientist, Dr. Lisa Feldman Barrett explains, “If you are daily coming into contact with a boss, a teacher, a coach, or even a colleague or peer who bullies you, your brain predicts that the situation is one of fight, flight, or freeze and this causes your body to release the stress hormone cortisol more often and in greater amounts than you need. This is a prolonged case of the body budget being out of balance.”
In other words, past experiences create our brain’s predictions on how to handle issues of today. That is why we don’t all experience stress the same way and if we don’t change these predictions and work on the inflammation it causes, motivation to eat well, exercise, and the ability to sleep well can all be compromised greatly leading to more health issues, especially mental health.
So, how can we slowly start to do exercises and actions to improve these qualities?
Research has shown quite a bit that mind-body practices that are part of our Myofascial Integrated Movement system help reduce inflammation and many of the other issues such as depression, anxiety, and overall regulation (2, 3). One paper in particular states, “Meditation allied strength, endurance, flexibility and enables self-control to create an awareness of concentration, calmness, relaxation, and well-being, presenting both physical and mental health benefits.” (2)
View this post on Instagram
Coach Cory Cripe does a great job showing how we use mindfulness, breath, and movement all together to start building these processes into programs that also provide fitness benefits.
Another paper on inflammation shares, “There is a growing literature examining effects of MBTs on inflammatory processes, reflecting increasing use of these approaches and recognition of the importance of inflammation for physical and mental health. Results from this review suggest that effects of these approaches may initially be reflected in alterations in gene expression profiles and indicators of proinflammatory signaling; indeed, alterations in inflammatory gene expression were identified even after relatively short (6 week) interventions (Bower et al., 2015) and generally appeared to be driven by reduced proinflammatory gene expression in the monocyte population. Studies examining cellular markers of inflammation also suggest that monocytes may be particularly sensitive to effects of MBTs, with effects on monocyte production of proinflammatory cytokines observed as early as 8 weeks after intervention onset.” (3)
What you can see below is when we get proficient in the foundations these movements start blending mobility, stability, strength, conditioning, and moving meditation all together.
You can learn more saving 25% off our online Masterclasses like our Low Back and Myofascial Integrated Movement classes HERE and also get 2 corrective exercise programs for FREE with code “online”
References:
- Dantzer R. Cytokine, sickness behavior, and depression. Immunol Allergy Clin North Am. 2009 May;29(2):247-64. doi: 10.1016/j.iac.2009.02.002. PMID: 19389580; PMCID: PMC2740752.
- Zeidan F, Martucci KT, Kraft RA, Gordon NS, McHaffie JG, Coghill RC. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011 Apr 6;31(14):5540-8. doi: 10.1523/JNEUROSCI.5791-10.2011. PMID: 21471390; PMCID: PMC3090218.
- Bower JE, Irwin MR. Mind-body therapies and control of inflammatory biology: A descriptive review. Brain Behav Immun. 2016 Jan;51:1-11. doi: 10.1016/j.bbi.2015.06.012. Epub 2015 Jun 23. PMID: 26116436; PMCID: PMC4679419.
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.