Why Fitness & Physical Therapy Struggle to Help Chronic Pain
2024-10-30
If there’s one roadblock that both clients and coaches consistently face, it’s dealing with chronic pain. People tell us their biggest barrier to making progress in training is pain. Coaches repeatedly ask how to help clients who feel limited by chronic pain. The struggle makes sense: pain can hinder consistency, cause hesitation, and make progress feel impossible.
Here’s the hard truth: pain is complex. Addressing it isn’t straightforward, and more than one thing can be true about it at the same time. From my experience and extensive interactions with professionals in both fitness and physical therapy, traditional approaches often fall short when it comes to managing chronic pain. But don’t just take my word for it. Look at pain statistics, research studies, and listen to people who struggle with it daily. My goal isn’t to share opinions but to explore what the most current science says about chronic pain. Let’s break down how pain works and why it’s so difficult to treat effectively in fitness and therapy settings.
Understanding Chronic Pain: What Does It Really Mean?
When we talk about chronic pain, it doesn’t necessarily mean feeling pain 24/7. Instead, it could be that every time you do a specific activity, pain flares up. Chronic pain typically refers to pain that lasts more than three months, and that distinction from acute pain (temporary pain that often resolves on its own) is crucial. Acute conditions, like low back pain, often improve with minimal intervention within three months. In fact, 90% of low back pain cases resolve during this acute phase simply by avoiding activities that aggravate the condition (1). However, once pain persists beyond this acute phase, it tends to take on a life of its own.
How Does Chronic Pain Take Root?
Interestingly, researchers have found that the risk of developing chronic pain isn’t determined by imaging of body structures but by brain activity. Studies can now predict with up to 85% accuracy who is likely to develop chronic pain within just three days of the onset of symptoms (2,3).
Why?
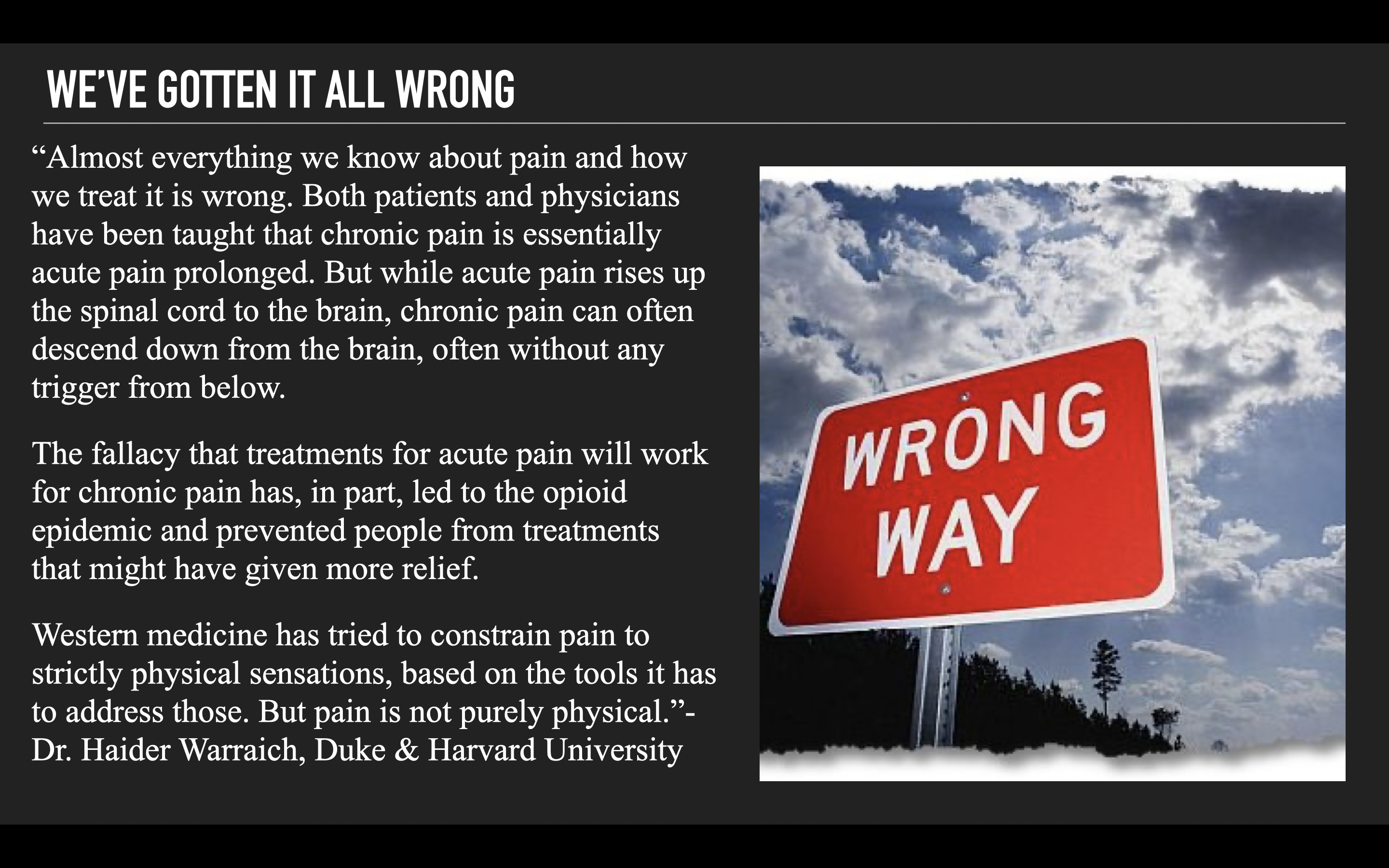
According to Dr. Apkarian, a leading researcher in this field: “The injury itself isn’t enough to explain ongoing pain. It’s about how the injury interacts with the state of the brain.” The more intensely the brain responds emotionally to an injury, the more likely it is for pain to persist beyond the healing period. Some people may have brains that are inherently more reactive, due to genetic or environmental factors, making chronic pain more likely.
But here’s what’s essential to understand: this doesn’t mean people are “imagining” their pain or that they’re “crazy.” Pain is always real. It’s just that the cause may not always be something wrong in the body’s structure. Pain, ultimately, is created in the brain, and when brain activity misinterprets body signals, it can become “stuck” in a pattern of chronic pain. Explaining this can be tricky, and it’s vital to approach it with empathy and clarity.
Two Key Brain-Based Pain Triggers
So, what keeps pain going, even when physical healing is complete? Here are two primary mechanisms:
1. Fear of Movement (Kinesiophobia):
When someone associates a movement with pain, the brain registers that movement as dangerous. This fear-avoidance response can make even low-intensity sensations feel unbearable, leading to a vicious cycle where the person avoids activities to prevent pain, which in turn creates inactivity, further disability, and greater sensitivity to pain (4).
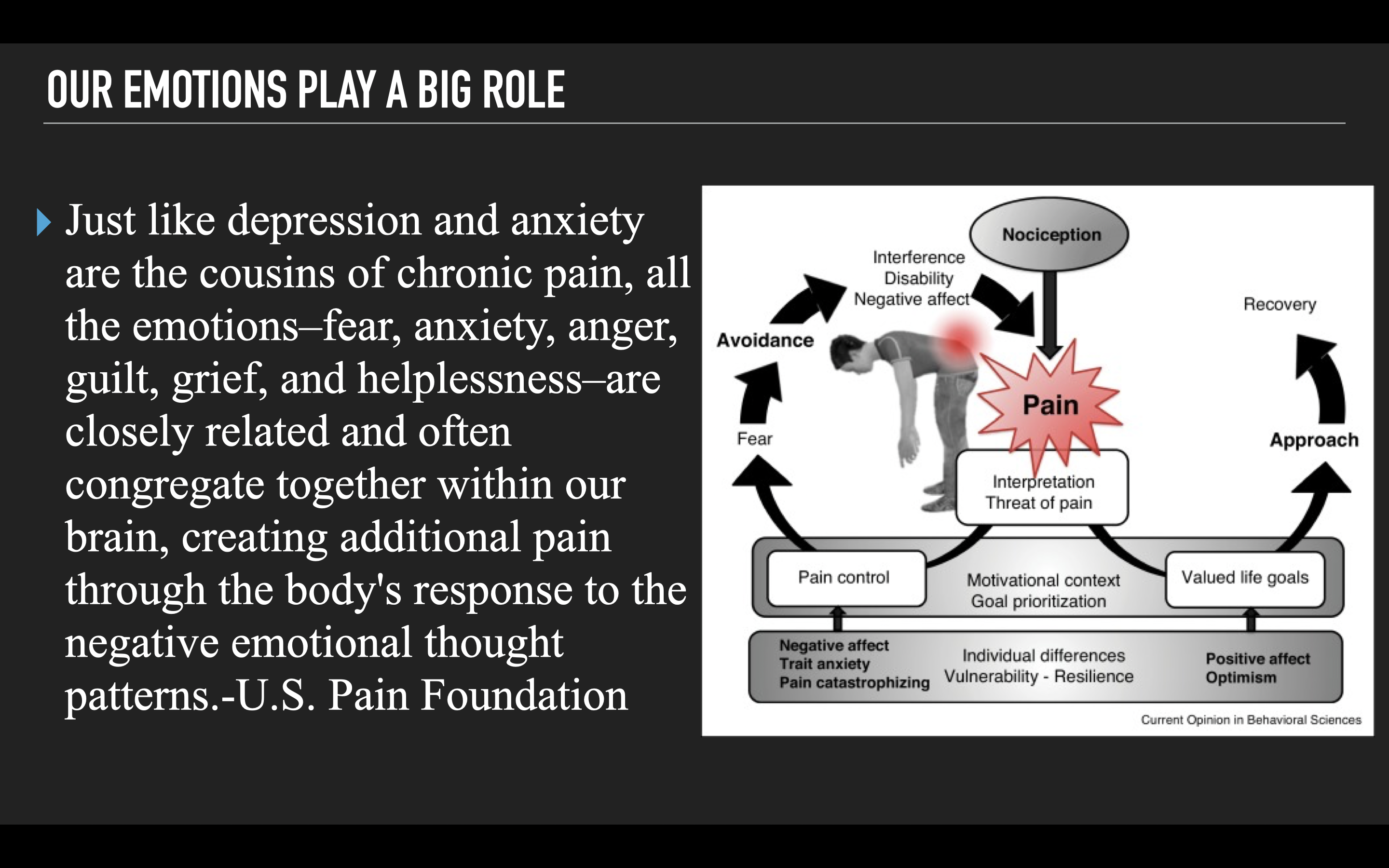
2. Predictive Coding:
This refers to the brain learning to anticipate pain based on past experiences. If a specific movement led to pain in the past, the brain might “predict” pain and generate pain signals whenever that movement is attempted, regardless of actual injury. This isn’t something people consciously do; it’s a protective response from the brain that can be difficult to break.
Moving Beyond Traditional Approaches to Chronic Pain
Contrary to popular belief on social media, current medical recommendations align closely with principles like those in the Myofascial Integrated Movement (MIM) system. Organizations such as the U.S. Department of Defense, Harvard Medical School, and The Arthritis Foundation endorse meditative movement practices to help with chronic pain. So, why is the fitness and physical therapy world slow to adopt these practices?
Studies show that meditative movement practices can reduce pain catastrophizing, a major source of emotional distress that fuels chronic pain. These practices are backed by research that shows they help improve a wide variety of chronic pain conditions (5,6). Regular engagement with mindful movement can even lead to changes in the brain, reducing both physical and emotional pain responses (7,8).
View this post on Instagram
Key Strategies for Implementing Pain-Relieving Movement Practices
To effectively incorporate these practices, here are some essential tips:
– Slow It Down: Rushing through exercises can worsen technique and intensify pain. Slowing down helps clients tune into how their bodies move, allowing them to become more aware of their body and let go of self-judgment.
– Focus on a Few Exercises: Limit the routine to 3–5 exercises in a circuit style. This keeps the focus on presence and allows people to move in ways that reduce their fear of movement.
– Keep Repetitions Low: Fewer, slower reps are usually more effective. The goal isn’t fatigue; it’s intention. Moving mindfully allows for greater intensity without overwhelming the body or brain.
Chronic pain may be complex, but a science-backed approach that respects the brain’s role can make a real difference. Check out the series below to see how physical therapist Jessica Bento and I discuss common pain misconceptions and strategies that can help.
Check out a workout from our NEW follow along Myofascial Integrated Movement (MIM) program below and see how we implement these strategies. Save 30% on this program and other MIM programs with code “mim30” HERE
References
1.Chiodo AE, Bhat SN, Van Harrison R, et al. Low Back Pain [Internet]. Ann Arbor (MI): Michigan Medicine University of Michigan; 2020 Nov. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572334/
- Branco, P., Bosak, N., Vigotsky, A.D. et al. Hippocampal functional connectivity after whiplash injury is linked to the development of chronic pain. Nat. Mental Health (2024). https://doi.org/10.1038/s44220-024-00329-8
- Baliki MN, Petre B, Torbey S, Herrmann KM, Huang L, Schnitzer TJ, Fields HL, Apkarian AV. Corticostriatal functional connectivity predicts transition to chronic back pain. Nat Neurosci. 2012 Jul 1;15(8):1117-9. doi: 10.1038/nn.3153. PMID: 22751038; PMCID: PMC3411898.
- J Orthop Sports Phys Ther 2016;46(2):38–43. doi:10.2519/jospt.2016.0601
- Hall AM, Kamper SJ, Emsley R, Maher CG. Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement Ther Med. 2016 Apr;25:61-6. doi: 10.1016/j.ctim.2015.12.013. Epub 2016 Jan 2. PMID: 27062950.
- Kong LJ, Lauche R, Klose P, Bu JH, Yang XC, Guo CQ, Dobos G, Cheng YW. Tai Chi for Chronic Pain Conditions: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sci Rep. 2016 Apr 29;6:25325. doi: 10.1038/srep25325. PMID: 27125299; PMCID: PMC4850460.
- Wu K, Li Y, Zou Y, Ren Y, Wang Y, Hu X, Wang Y, Chen C, Lu M, Xu L, Wu L, Li K. Tai Chi increases functional connectivity and decreases chronic fatigue syndrome: A pilot intervention study with machine learning and fMRI analysis. PLoS One. 2022 Dec 1;17(12):e0278415. doi: 10.1371/journal.pone.0278415. PMID: 36454926; PMCID: PMC9714925.
- Xie, H., Zhang, M., Huo, C. et al. Tai Chi Chuan exercise related change in brain function as assessed by functional near–infrared spectroscopy. Sci Rep 9, 13198 (2019). https://doi.org/10.1038/s41598-019-49401-9
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.