Ozempic, Weight Loss, and the Missing Piece: Why Behavior Still Matters
2025-09-28
Jessica Bento, Physical Therapist (Don’t Miss 25% Off Our Fat Loss 6-week CEU Masterclass HERE)

In just the past few months, I’ve noticed how quickly weight loss drugs like Ozempic have become part of everyday conversations. For example, when I was out with some girlfriends, one of them brought up another friend (who wasn’t with us) and commented on her “unfortunate” weight gain. She couldn’t understand why that friend wouldn’t just “take the shot.” More recently, while spending time with a different group of friends, I heard a similar comment: “If you want to lose weight, I don’t know why you don’t just take the shot!”
The ease and casualness with which people suggest these drugs really struck me and, honestly, made me feel uneasy. It left me thinking that this is a conversation worth having. I want to share some information I believe is important for people to know, especially since I’m sure I’m not the only one who has found themselves in these kinds of situations.
Ozempic and similar GLP-1 medications have quickly become some of the most talked-about treatments for weight loss. Originally developed for managing type 2 diabetes, these drugs reduce appetite and improve blood sugar control, which naturally leads to lower calorie intake and weight loss. The results are often impressive, especially for people who have struggled with weight for years despite trying traditional diets. But as promising as these medications are, they are not without drawbacks—and long-term success still depends on behavior and lifestyle.
The Problem of Muscle Loss
One of the most concerning findings about Ozempic and other GLP-1 medications is their impact on body composition. Weight loss is not just fat loss; it often includes lean body mass—muscle, water, and organ tissue. Research shows that muscle loss with these drugs ranges from 25% to 39% of the total weight lost over 36–72 weeks (PMID: 38829659).
This matters because muscle isn’t just about strength or appearance it plays a critical role in metabolic health. Muscle tissue burns more calories at rest than fat tissue, helps regulate blood sugar, and protects against age-related frailty. Losing too much muscle during weight loss can lower metabolism, making it easier to regain weight once medication is stopped.

Plateaus Are Normal
Even with continued use, the benefits of Ozempic don’t last forever. As Dr. Ali from Memorial Care Surgical Weight Loss Center explains, “patients tend to plateau with semaglutide at 60 weeks. So it’s over a year, which is pretty good.”
This plateau is a reminder that the body adapts. Over time, appetite regulation shifts, and the initial dramatic weight loss slows down. Without behavior changes in place like exercise, meal planning, and stress management many people find themselves stuck at a plateau or sliding backward.

What Happens When You Stop?
Perhaps the biggest challenge with Ozempic is what happens when people discontinue the drug. A randomized-controlled trial found that one year after stopping semaglutide, participants regained two-thirds of the weight they had lost(PMID: 37513906). That’s a significant rebound effect, and it raises questions about whether these medications are best viewed as long-term, even lifelong, treatments rather than short-term fixes.
Some of this weight regain may be tied to the brain’s reward system. GLP-1 medications reduce food cravings and the drive to eat for pleasure. Once the medication is stopped, those reward circuits can reactivate, making cravings feel stronger than before.

Why Behavior Still Matters
All of this underscores an important truth: medication can be a powerful tool for weight loss, but it cannot replace healthy behaviors. The most successful long-term weight loss strategies focus on protecting muscle, managing cravings, and building sustainable habits. Fortunately, research points to several evidence-based strategies that make a real difference.
1. Strength Training to Preserve Muscle
If 25–39% of weight lost on Ozempic is lean mass, then protecting muscle should be a priority. Studies consistently show that resistance training preserves fat-free mass during weight loss. Even two to three sessions per week of bodyweight, resistance bands, or weightlifting can reduce muscle loss and help maintain metabolism. Pairing strength training with adequate protein intake (1.2–1.6 g/kg of body weight per day) further protects lean tissue.
Realize though when someone is severely calorically restricted, as is often the case with GLP-1 drugs they can cause people to feel more fatigued and impede recovery. You can’t give people on such medications a crazy intense workout as they don’t have the fuel to recover from such training.
2. Mindful and Structured Eating
GLP-1 medications help people eat less by reducing hunger and cravings. But once the drug is stopped, old habits often return. This is where mindful eating practices come in. Research shows that mindful eating helps people recognize true hunger, slow down during meals, and reduce emotional or binge eating (PMID: 20046886). Structured meal planning like preparing balanced meals ahead of time can also reduce decision fatigue and prevent impulsive choices.
3. Stress Management
Chronic stress raises cortisol, which increases cravings for high-calorie foods and promotes fat storage. Stress management strategies such as meditation, journaling, breathwork, or even short daily walks—have been shown to lower cortisol and improve self-regulation. This isn’t just about “feeling better.” Stress resilience helps prevent the rebound eating that often follows medication withdrawal.
This is why programs like our Myofascial Integrated Movement system can be such a powerful addition to any program. Such movements don’t just help with our mobility, but research shows that it can help us manage the emotions that cause us to reduce our ability to stay on track and avoid emotional eating habits.
4. Reframing Success Beyond the Scale
Finally, one of the best behavioral strategies is shifting the focus from weight alone to overall health behaviors. Regular physical activity, balanced nutrition, adequate sleep, and nervous system regulation improve health even if the scale doesn’t move dramatically. This reduces the frustration of plateaus and helps people stick with habits that matter in the long run.
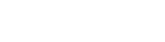
Focusing more on a growth mindset where we look at our ability to implement habits and avoid absolutes can great improve adhere and motivation to any fitness goal.
The Bottom Line
Ozempic is not a magic bullet. It can help kickstart weight loss, reduce appetite, and improve metabolic health, but it comes with trade-offs: significant muscle loss, inevitable plateaus, and high rates of weight regain after stopping. The key to long-term success isn’t choosing between medication and behavior it’s understanding the true underlying keys of the obstacles one facets. In some cases medications will be necessary, but even then, we still need to help people better understand the impact of behavioral modification for the long run.
Learn so many MORE strategies in our upcoming “Why Fitness Has Failed Fat Loss” 6-week online CEU Masterclass starting October 28th. You can save 25% on the masterclass THIS week only with code “coach25” HERE
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.