The Hip Mobility Mistake Almost Everyone Makes
2026-02-16
Mobility has NEVER been my thing!!! I remember when I started working out as a 14 year old I just felt stiff and that is why I often defaulted to using machines many times when I began training. Over the years, building better mobility has really been a goal of mine, however, it hasn’t been an easy journey.


yea, my spine isn’t a pretty picture
Especially because for the past 35 years I have also battled an aggressive degenerative disease in my spine. That has made my hips particularly a point of great mobility despair. However, it has opened my eyes to SOOOO many ideas and programs around mobility. In fact, I would pretty much say, if there has been a program based around improving mobility I have dove into looking into the programs.
That is why when I now write this post, I can summarize what actually works in improving hip mobility (okay, not just hip mobility), to a few key points.
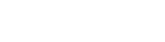
The Overlooked Impact Of Nerve Glides
Research shows that peripheral nerves are not static structures they must slide and adapt to movement. The sciatic nerve, for example, travels from the lower back through the hip and down the leg. During hip flexion, extension, and rotation, the nerve needs to glide relative to surrounding muscles and fascia. If neural mobility is restricted, the nervous system may increase protective muscle guarding, creating the sensation of “tight hips” even when muscle length isn’t the primary limitation.
Studies on neural mobilization demonstrate improvements in range of motion and reductions in pain sensitivity, likely due to decreased mechanosensitivity and improved intraneural blood flow. By gently tensioning one end of the nerve while slackening the other, nerve glides promote movement without excessive strain, reducing threat perception within the nervous system.
When neural sensitivity decreases, the body often allows greater hip range because it no longer perceives the movement as unsafe. In this way, nerve glides don’t just stretch tissue they improve communication between the nervous system and the musculoskeletal system, allowing hip mobility to improve more comfortably and sustainably.
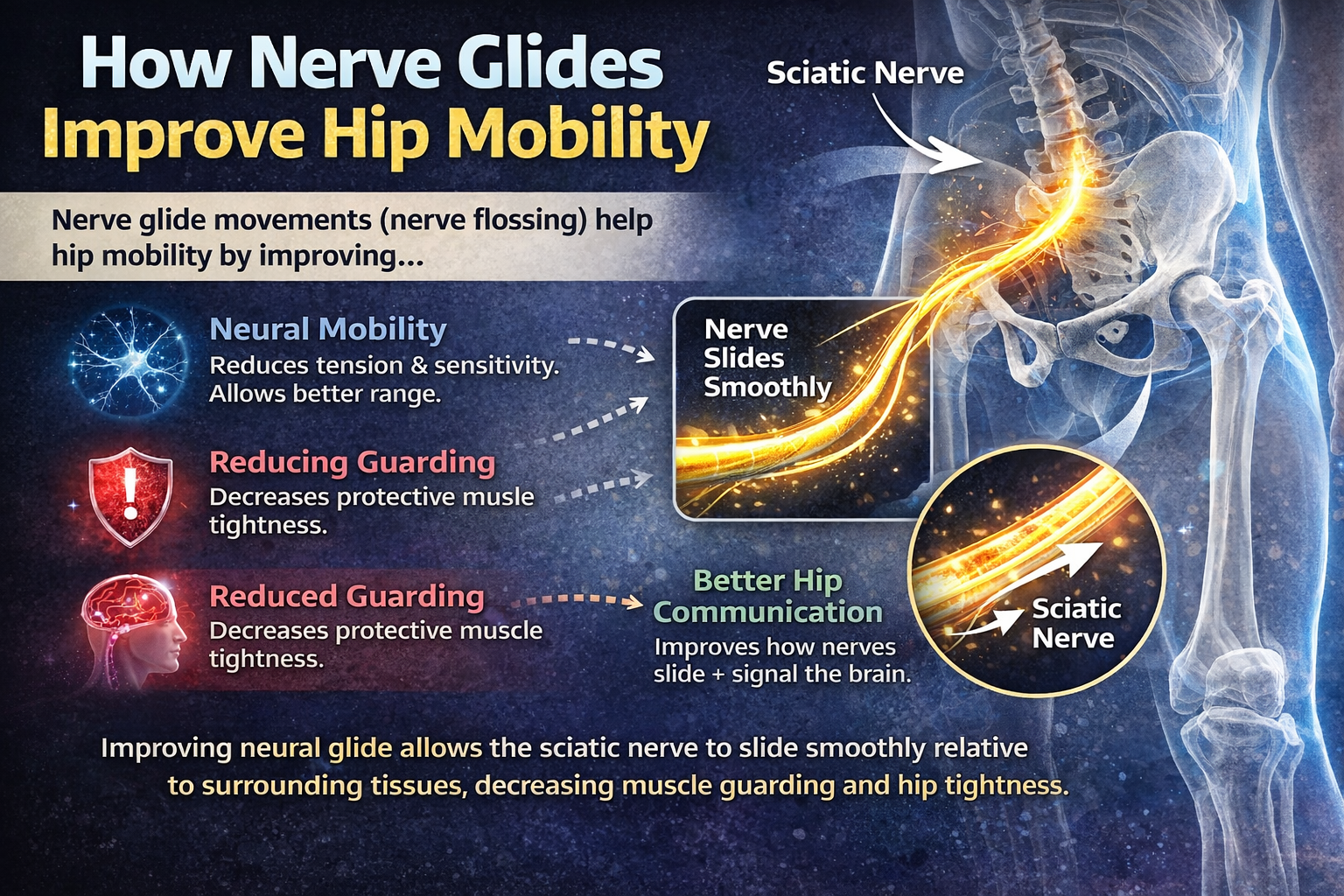
The Core Is REALLY Important!
Research consistently shows that proximal stability is a prerequisite for distal mobility, especially at the hip. The hip is a highly mobile ball-and-socket joint, but its ability to move efficiently depends on adequate stability from the trunk and pelvis. When the core and lumbopelvic stabilizers are not functioning well, the body often limits hip motion as a protective strategy.
Studies examining lumbopelvic control demonstrate that poor trunk stability is associated with altered hip kinematics, increased compensatory lumbar motion, and higher risk of lower extremity injury. When the deep stabilizers; including the transversus abdominis, multifidus, diaphragm, and pelvic floor, fail to provide sufficient control, the nervous system reduces available range at the hip to maintain safety. In other words, what looks like “tight hips” is often a stability issue rather than a true mobility restriction.
Additionally, research in athletic and clinical populations shows that improving proximal strength and neuromuscular control can enhance hip range of motion without aggressive stretching. Strengthening the gluteals, lateral hip stabilizers, and trunk musculature improves joint centration and reduces compensatory patterns.
True hip mobility is not just about flexibility. It is about owning motion with control. Without proximal stability, mobility becomes instability and the body will always choose protection over performance.
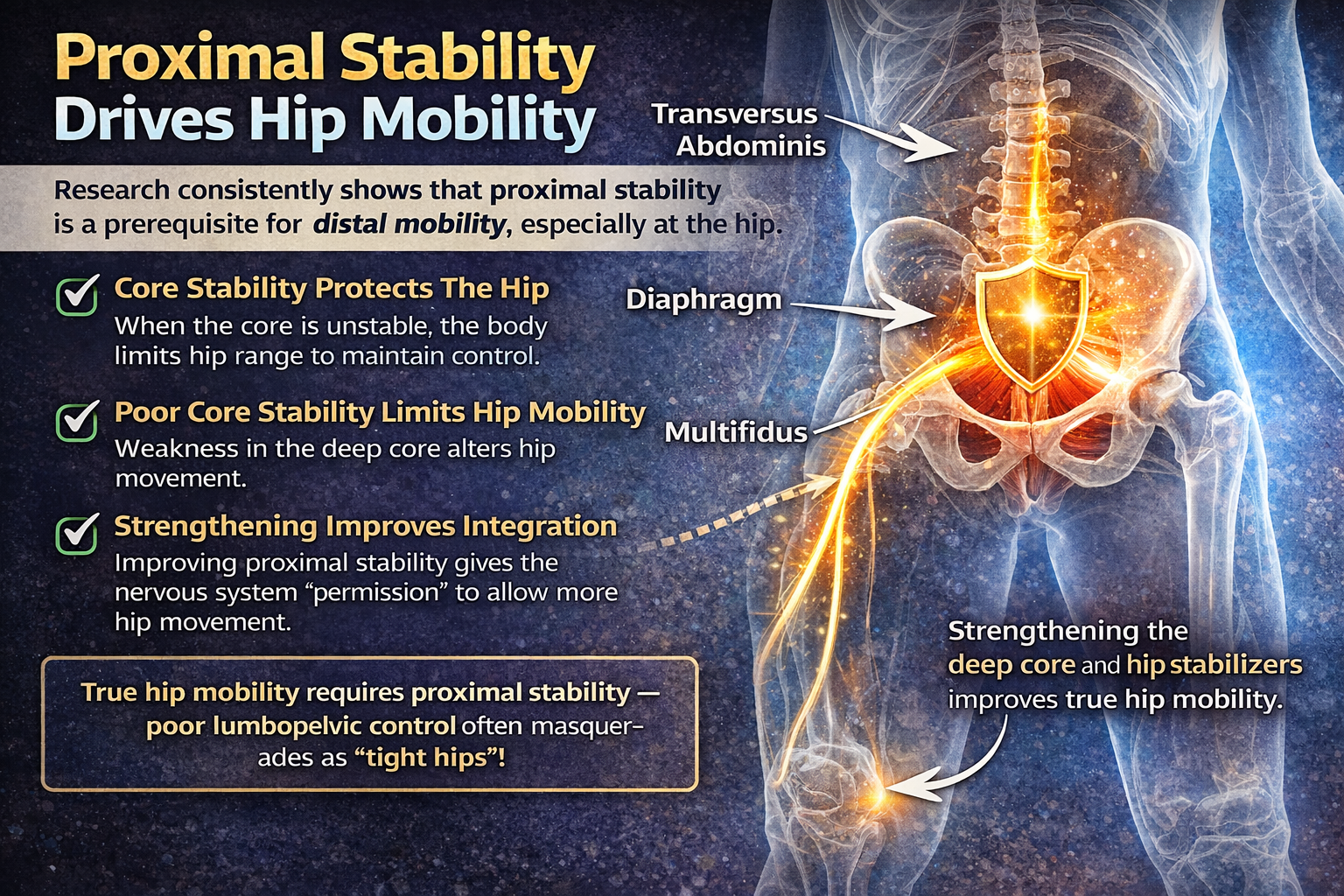
The Nervous System & Kinetic Chain
Research consistently shows that hip mobility is not just a local flexibility issue, but a systems issue involving both the kinetic chain and the nervous system.
From a biomechanical perspective, the hip functions within an integrated chain linking the feet, pelvis, trunk, and shoulders. Studies on lumbopelvic control demonstrate that poor trunk stability is associated with altered hip mechanics and increased compensatory lumbar motion. When proximal stability is insufficient, the nervous system often restricts distal motion as a protective strategy. Training the kinetic chain, through coordinated, multi-joint movements that integrate the glutes, deep core stabilizers, and lateral hip musculature, improves joint centration, force transfer, and neuromuscular control. Research in both athletic and rehabilitation settings shows that improving proximal strength can increase available hip range of motion without aggressive stretching.
At the same time, a dysregulated nervous system can elevate muscle tone and increase threat perception, leading to guarding around the hip. Chronic stress and pain sensitivity are associated with heightened sympathetic activity and reduced movement variability. Interventions that enhance parasympathetic regulation , such as breathing strategies, graded exposure to movement, and controlled mobility drills, reduce mechanosensitivity and improve motor control.
When kinetic chain integrity and nervous system regulation improve together, the body no longer needs to “protect” the hip. Mobility becomes something the system allows, not something forced.
NOTHING is magical and EVERYTHING takes consistent effort that can be influenced by fatigue, stress, injury, and a host of other factors. If we follow these principles we can always find a progression or a solution for what you need at that time and that is the goal. Exercises may change, but for principles will always be our guide. That is. why I wanted to give you some practical examples below…
Find out SO much more at our upcoming “Fitness Over 40” FREE Webinar Tuesday Feb. 24th HERE
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.