Why Fascial Training Does Matter
2024-07-19
Over 10 years ago I wrote my first article about fascial training (I’ve written several for different outlets since). It became one of my most popular because most of the fitness world had never heard of fascia and I think I did a decent job sharing the science that makes fascial training something that fitness, performance, and even cosmetic training should understand (already being used in many therapeutic circles).
If you think fascial training discussions are just trendy new fitness concepts, this isn’t true at all. You can find discussions of fascia thousands of years ago in cultures like ancient Egypt and China, even though it wasn’t called fascia at the time. That is why we see references to fascial like training discussions in yoga, qigong, and Tai Chi practices.
In a great article about the history of fascia, we see the term fascia makes its first anatomical appearance under the Roman Empire with Galen of Pergamon using it to describe the attachment of muscles also known as ‘origins and insertions’. It is a Latin word derived from the Greek taenia and means ‘string of fabric’ (you can read more HERE). This is a very appropriate description since fascia moves throughout our body and serves many functions from our muscles and joints to organs and more!
A great article by fascial expert, Dr. Helen Langevin (Director of the National Center for Complementary and Integrative Health at the National Institutes of Health. She was a professor in the University of Vermont College of Medicine’s Department of Neurological Sciences. )
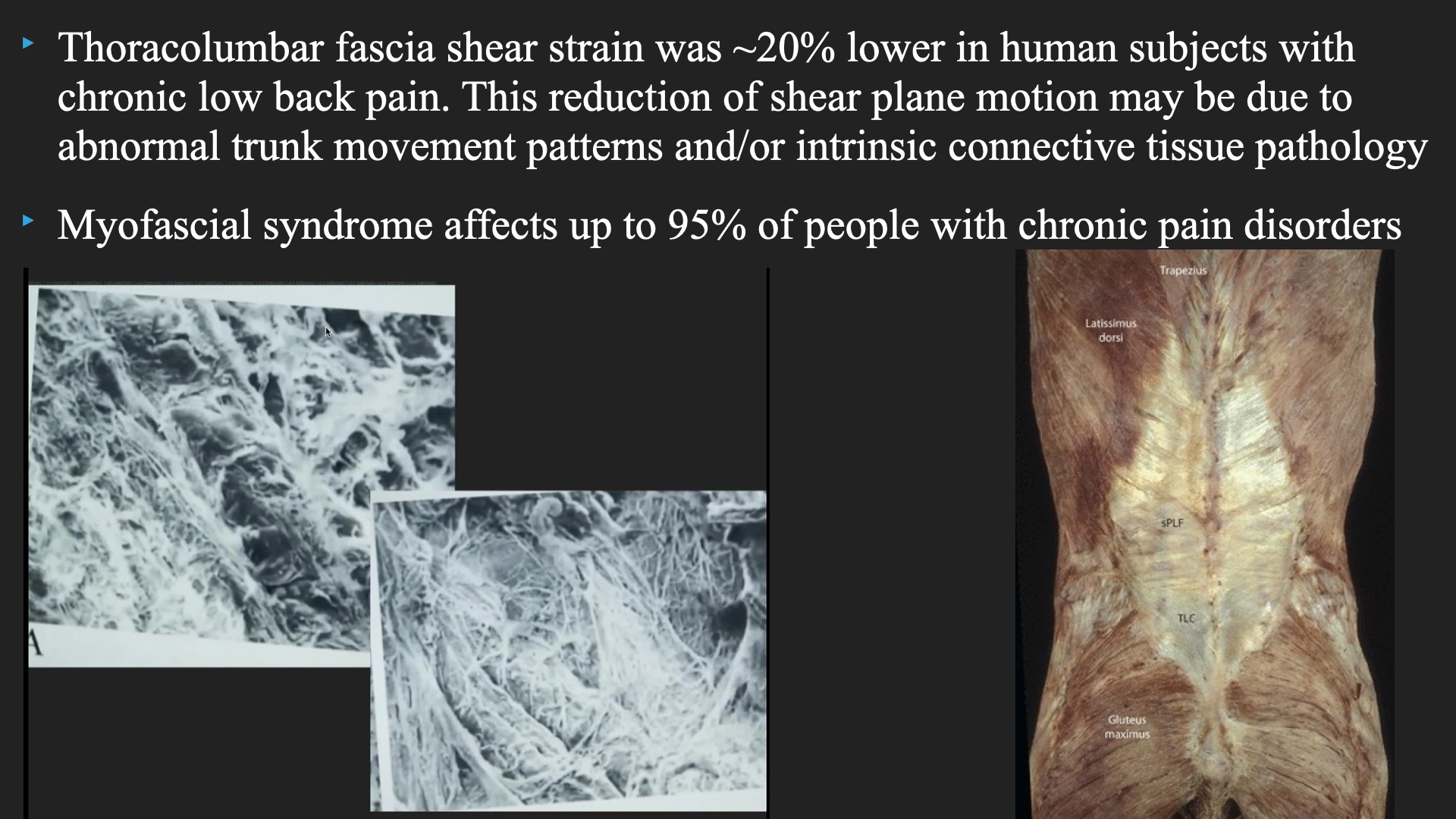
“Fasciae are composed of irregularly arranged but tightly woven connective tissue that can bear high tensile loads. Fascial planes are separated by planes of “loose” connective tissue that allows the fasciae to glide past one another. The motion between the fascia layers is a significant component of musculoskeletal mobility. When two adjacent layers become adherent, either due to scarring after an injury, or due to posture habits, some of the interfacial mobility is lost. The consequences of reduced fascia mobility on the function of muscles and joints are potentially profound but mostly unknown.
Furthermore, the sensory information derived from fasciae and its contribution to proprioception (internal “body sense”) and musculoskeletal pain is basically unstudied. This is because, historically, more attention has been given to specialized musculoskeletal tissues (i.e., bones, cartilage, intervertebral discs, muscle) than to “non-specialized” connective tissue, including fasciae, but this is beginning to change.

Although the clinical syndrome of “myofascial pain” remains poorly characterized, it is estimated to be present in approximately 30% of patients with chronic musculoskeletal pain in the back, neck, shoulder, hip, and pelvis as well as temporomandibular pain, and headache. Over the past two years, three National Institutes of Health (NIH) workshops have addressed these related topics to stimulate research: “Quantitative Evaluation of Myofascial Tissues”, “Neurocircuitry of Force-Based Manipulation”, and “The Science of Interoception and Its Roles in Nervous System Disorders” (1).
Now I recognize the above is A LOT to digest, but let me give you some important notes to realize.
-Fascial training and systems are real! Some try to question the value of fascial training and whether fascia is important in general. More and more research shows it is an essential aspect of how our bodies move, the sensations we experience, as well as other health issues.
-Pain and our mobility/flexibility have large fascial components. They aren’t everything, but they play an important part in both pain and mobility/flexibility. Most times when we stretch we are probably moving and placing more demands on the fascia that encapsulates muscle, than the muscles themselves.
We can also see that when we have pain, we can increase tension of our fascia, sometimes, reduced fascial movement can be related to increased pain (back pain is a common one), which is also why movement is an important tool in helping pain because when we don’t move, our cognitive tissue (fascia) starts to mold differently allowing for less freedom of movement. (2)
-Our body is one interconnected system. This not only means that all the muscles of our body are connected via these fascial systems, but so are the various systems of our body. Combining this with how our brain interacts with everything (including with our fascia) it only speaks to more and more why isolation of anything (mobility, strength, etc.) makes little sense in optimizing the body and why our focus should be on integrated strategies.
So, what does this all mean for your training? Is stretching good for your fascial training? It can be helpful. Is full body range of motion strength training helpful for your fascial training? Yup, that can help too. However, done without the right intent, these methods will hit their limitations in producing better movement of the fascia, because there are other factors at play. One more element that people have to understand, this is the more challenging aspect.
Our brain runs everything in our body and constantly has an interplay between mind and body. That means when we are dealing with really stressful times in our lives, if we are often an anxious person, if we are not learning how to manage our stress levels and events in life, then all the stretching and strength training may not resolve the issue. I know, you want to go to the gym and just train and I hear you, but you don’t have to go into intense emotional therapy to help (although in some cases may be appropriate).
A great 2017 paper explains, “Patients with myofascial pain commonly experience depression, sleep disturbance, anger, fatigue, and altered mental function. They frequently require an interdisciplinary approach to address the many dimensions of pain experience. Although medications are frequently advised, it is necessary to think of alternative therapies such as meditation. Meditation operates on a wide range of pain categories and can alleviate chronic pain in patients who do not respond to traditional medical care. Meditation works better than morphine in pain management.” (3)

That sounds absurd but research does show that over the long term, pain medications either stop helping or can make chronic symptoms worse while “re-wiring” your brain through meditation can be a big part in alleviating pain issues. Below, you can see how myofascial pain and our brain are so closely connected that we have to learn how to integrate strategies that NOT only help our body but also our brain.
Like I said, this can be done through training or at least greatly helped. Stressful events are part of life, but the issue is how we deal with them. So, if we can find practices that address some of these brain changes that happen with chronic pain and stress, we can start on the journey of making pain, movement, and even our strength better which is tapping not only into fascial training, but our neurology too!
That is why I created the Myofascial Integrated Movement system (MIM) using influences from yoga, Tai Chi, and qigong, which all have A LOT of research on fascial training, pain, and improved movement, and well-being to be more accessible to people who aren’t ready to do a deep dive into these systems and who also want to accomplish other goals at the same time. You can see this through how we put together MIM exercises in our workouts.
We can use these exercises as a whole workout, a warm-up, a way to get more movement into our daily routine, as corrective exercises, and more. So, don’t underestimate what these movements can accomplish as their benefits span a wide range.
Don’t miss the release of our NEW Mobility Training Balls HERE and when you email proof of purchase to info@ultimatesandbagtraining.com you will get 2 FREE in-depth training manuals to show you how effective this training can be!
References:
- Langevin, H.M. Fascia Mobility, Proprioception, and Myofascial Pain. Life 2021, 11, 668. https://doi.org/10.3390/life11070668
- Casato G, Stecco C, Busin R. Role of fasciae in nonspecific low back pain. Eur J Transl Myol. 2019 Aug 6;29(3):8330. doi: 10.4081/ejtm.2019.8330. PMID: 31579477; PMCID: PMC6767839.
- Panta P. The Possible Role of Meditation in Myofascial Pain Syndrome: A New Hypothesis. Indian J Palliat Care. 2017 Apr-Jun;23(2):180-187. doi: 10.4103/0973-1075.204239. PMID: 28503039; PMCID: PMC5412127.
© 2026 Ultimate Sandbag Training. Site by Jennifer Web Design.